Abstract
Introduction: Hemophagocytic lymphohistiocytosis (HLH) is a rare syndrome of excessive and ineffective activation of the immune system resulting in hyper-inflammatory response. Common presenting features include fever, cytopenias, elevated serum ferritin, and splenomegaly. HLH diagnosis is challenging as the available diagnostic criteria lack specificity. In addition, patients have a dismal outcome, and markers predicting survival are lacking. Ferritin concentration is a surrogate marker for inflammation, and repeated measurements might be associated with disease severity and outcome. We explored the prognostic significance of serum ferritin in adult HLH.
Methods: We reviewed diagnoses of adult HLH treated at Barnes-Jewish Hospital (St. Louis, Missouri) and Henry Ford Hospital (Detroit, Michigan). We included 98 patients who met the 2004 Histiocyte Society criteria for HLH and had at least 2 serial ferritin values during the admission when diagnosis was established. Admission ferritin was defined as the initial value, and peak ferritin was defined as the highest value during admission. We examined ferritin levels change during admission which could be increasing (peak ferritin being the last ferritin value) or decreasing (ferritin values decreasing after peak ferritin). Predictive factors for survival during hospital admission were evaluated by univariate analysis followed by logistic regression. Analyses were performed using SPSS version 22, and results were considered significant at p <0.05.
Results: The median age of patients was 48 years (range, 18-79 years); 64 (65%) were male. The most common clinical and laboratory abnormalities during hospitalization were: hyperferritinemia (100%; median 27,306 µg/L; range 1,823 - 684,000 µg/L), fever (96%), cytopenias (91%), hemophagocytosis (76.7%), elevated triglycerides (72.4%), splenomegaly (67.3%), and hypofibrinogenemia (42.7%). Median duration of hospital stay was 20 days (range, 1 - 89 days); 38 (39%) patients died during admission. Death was attributed to sepsis in 23 patients, lymphoma in 7, bleeding in 4, GVHD in 1, liver failure in 1, metastatic solid tumor in 1, and unknown in 1.
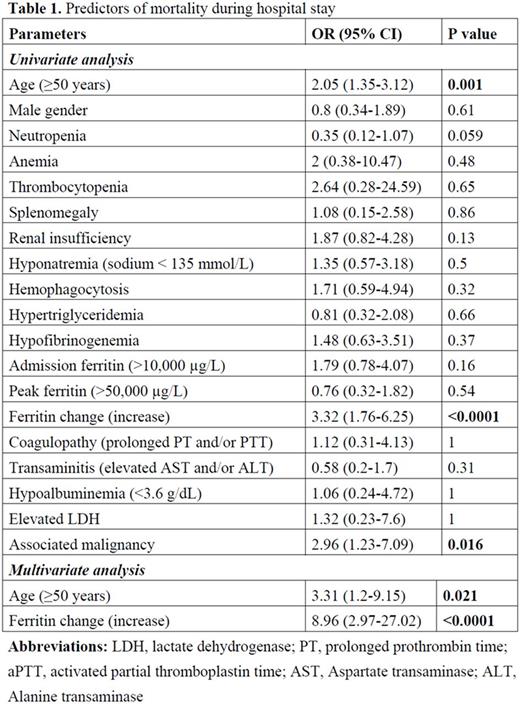
Table 1 shows the parameters analyzed as predictors of mortality during hospital stay. In the univariate analysis, we found that age ≥50 years, increasing ferritin levels during admission, and malignancy were associated with higher mortality. At the multivariate regression level, age ≥50 years (OR = 3.31; 95% CI: 1.2 - 9.15; p = 0.021) and increasing ferritin levels (OR = 8.96; 95% CI: 2.97 - 27.02; p <0.0001) correlated with mortality. In addition, patients with declining ferritin levels by more than 50% from the peak were more likely to survive (OR = 2.21; 95% CI: 1.13 - 4.3; p = 0.026).
Conclusion: Our results showed that ferritin trends rather than absolute concentration are associated with risks of mortality when HLH is diagnosed during a hospitalization. A declining ferritin trend is associated with lower risk of death and an increasing ferritin trend is associated with an increased risk of death. Prospective investigations of ferritin trends in HLH are warranted.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.